Case Study
Topic : Ametropia Management of presbyopic and mixed & compound Hyperopic astigmatism with progressive additional lens.
By Dr.Loft,O.D.
public : 4 September 2024
Case History
Patient Information:
Ms. Cecilia ,age 66 years old ,female
Reason for Visit: Routine check-up
Case History:
Ms. Cecilia had lens replacement 5 years ago (14 Nov 2019), but the coating on her current lenses has started to deteriorate, and she wants new lenses. If the coating issue is ignored, the old lenses still function well for both distance and near vision. However, when she covers one eye, she notices that her left eye has become blurrier than the right. She is currently on a one-month vacation in Thailand and took this opportunity to get her lenses checked and replaced.
Previous Examination (14 Nov 2019):
Age at that time: 61 years old
Issues: Blurred vision at both distance and near. She had progressive lenses but couldn’t wear them comfortably, despite multiple adjustments at an optical store in Singapore. Before visiting the Loft Optometry clinic, she researched and decided to undergo an eye examination during her vacation in Thailand.
Clinical Findings:
The primary issues were refractive error and presbyopia, and the previous lenses did not provide full correction, causing discomfort. However, the binocular function of the eyes was normal. The refraction values and lenses prescribed at that time were:
Refraction:
Right Eye (OD): +2.75 -2.00x93, VA 20/15
Left Eye (OS): +2.50 -2.00x93, VA 20/15
Add: +2.00
Lens Rx : Rodenstock Multigressiv MyView 1.6, L
Initially,
The patient was concerned that she might not be able to wear the new lenses, as she had to return to Singapore soon and had already spent a lot of money on previous attempts (according to the patient). She opted for mid-range lenses and kept her old frame, deciding that if she couldn’t wear them, she wouldn’t regret the expense. So,I made new lenses for her using her existing Silhouette frame.
After receiving the glasses,
The patient was able to wear them immediately without any issues. She mentioned that initially, her iPad screen appeared slightly distorted, but this resolved within two days.
Three years later,
She saying the coating was deteriorating and she wanted new lenses. But Due to the COVID-19 pandemic, traveling between countries was difficult, so she continued using her old glasses until one of the arms broke. She then tried to have new glasses made locally in Singapore, but they still didn't work well, even though the optical shop tried to match the old lenses (from the broken pair). The patient said that none of the new glasses worked, despite trying several shops. The shop eventually suggested buying a new Silhouette frame (same model) and transferring the old lenses to it.
Recent Examination (3 Aug 2024):
The patient visited the clinic again during her vacation in Thailand to have new glasses made. The refraction values obtained are as follows:
Refraction:
Habitual Rx (old glasses):
OD: +2.75 -2.00x93 VA 20/25+2
OS: +2.50 -2.00x93 VA 20/30
Retinoscopy:
OD: +3.00 -2.00x90 VA 20/20
OS: +2.00 -2.25x90 VA 20/20
Monocular Subjective Refraction:
OD: +2.75 -2.50x102 VA 20/20
OS: +2.00 -1.87x90 VA 20/20
Best-Corrected Visual Acuity (BVA, on-phoropter):
OD: +2.75 -2.50x102 VA 20/20
OS: +2.00 -2.00x93 VA 20/20
Best-Corrected Visual Acuity (BCVA, fine-tuning on trial frame):
OD: +2.75 -2.50x102 VA 20/15
OS: +2.00 -1.87x95 VA 20/15
VAOU 20/15+2
Binocular Function: Normal
BCC: +2.0
NRA/PRA: +0.75/-0.75, relying on BCC
Assessment:
- Mixed hyperopic astigmatism in the right eye (OD), compound hyperopic astigmatism in the left eye (OS).
- Presbyopia.
- Normal binocular function.
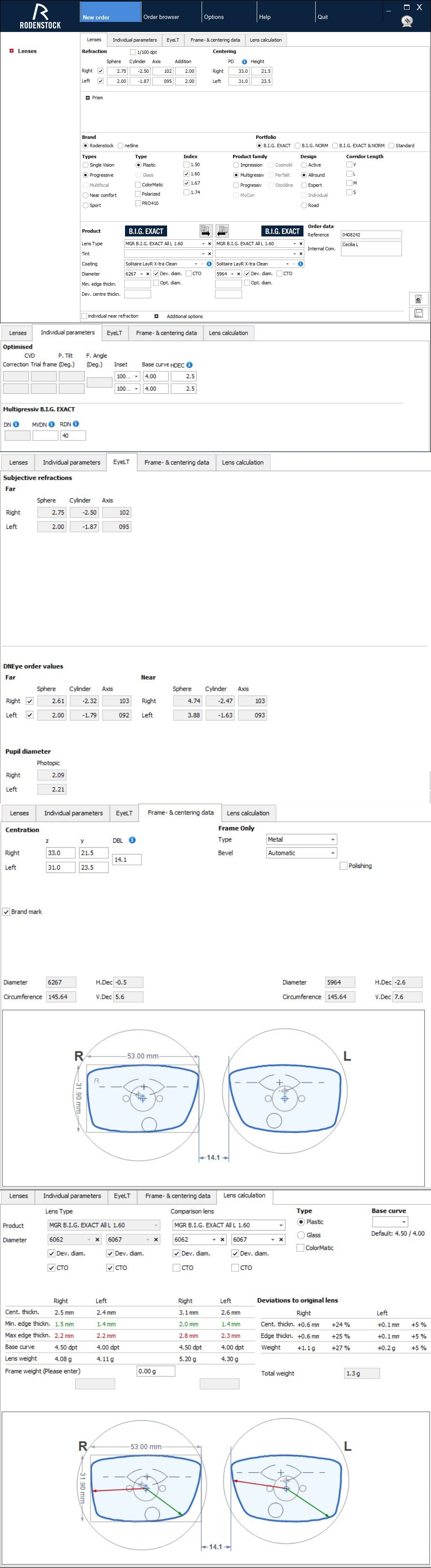
Plan:
- Full Rx:
OD: +2.75 -2.50x102
OS: +2.00 -1.87x95
- Progressive lens prescription with Add +2.00: Rodenstock MGR B.I.G. Exact 1.6, Allround, L.
- N/A
Discussion:
Refractive Change:
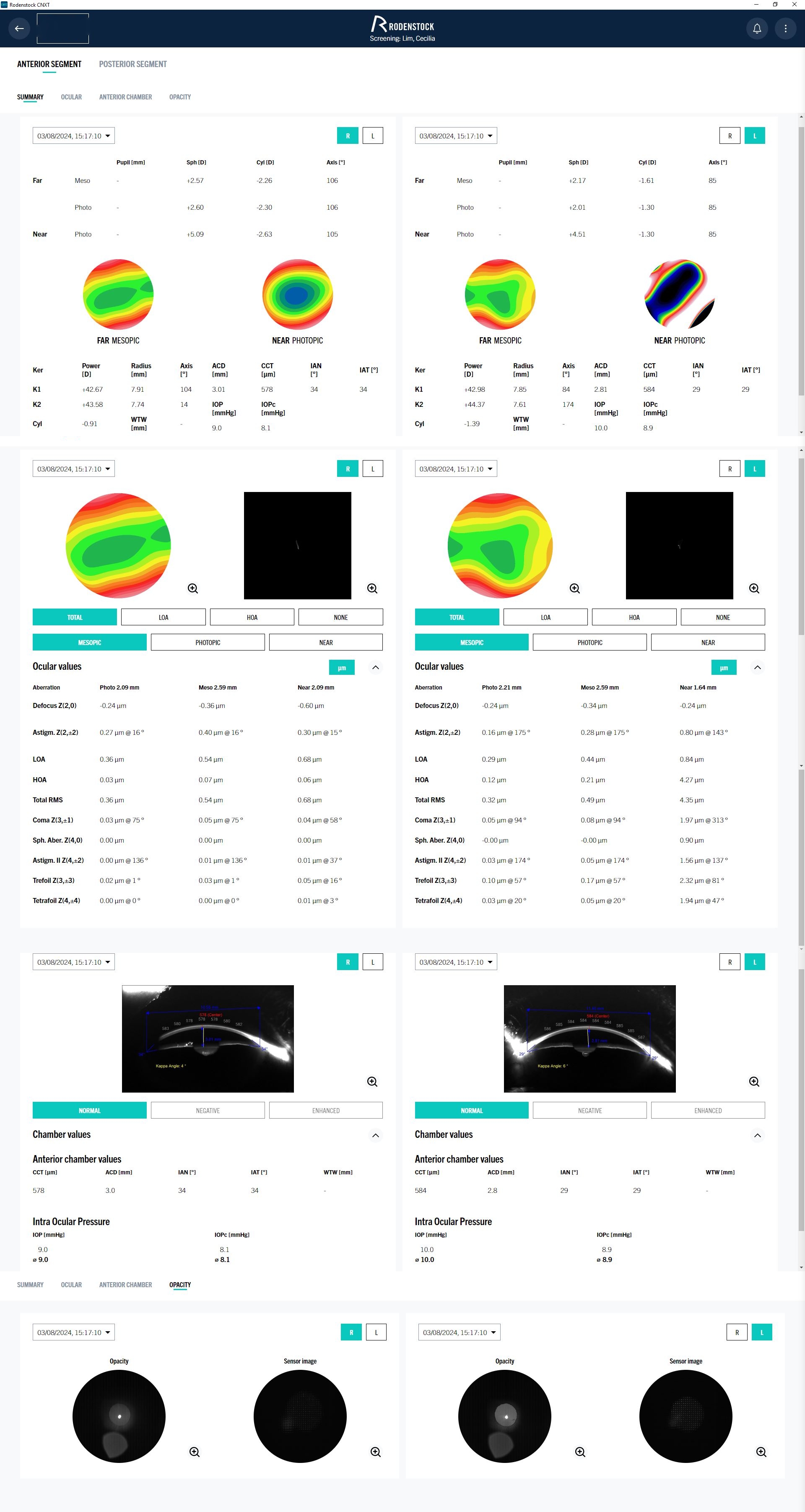
The patient’s overall refractive status has remained almost stable, with a noted reduction in hyperopia in the left eye, likely due to early cataract changes. However, the corrected vision remains sharp (VA 20/15). It will likely take years before the cataract progresses to the point of affecting vision quality.
Presbyopia:
Presbyopia occurs due to the decreased flexibility of the lens, leading to the inability to accommodate for near vision. As a result, the eye muscles strain without achieving focus, causing blurry near vision. To compensate, we use lenses with positive power to assist with near focus as the natural lens loses its ability to accommodate.
Early Sign of Cataracts:
A common early sign of cataracts is a lower than average BCC (or Add value). Typically, a 66-year-old patient would have an average Add value of +2.50D to +2.75D, but in practice, it's rare to see an Add value as high as +2.50D. In cases I’ve handled, the Add often caps at +2.25 or lower. This can be explained by early structural changes in the lens due to cataracts, an effect historically referred to as "second sight (Sometimes, a cataract may temporarily improve a person's ability to see close-up, because the cataract acts as a stronger lens. This phenomenon is called second sight, because people who may have once needed reading glasses find that they don't need them anymore. (ref : https://www.webmd.com/eye-health/cataracts/ss/slideshow-cataracts )"
Therefore, when testing elderly patients, if the Add value exceeds +2.25D, it’s worth considering the possibility of over-minus or under-plus prescription, often due to uncorrected residual astigmatism. In such cases, the patient might accommodate to make the circle of least confusion (the sharpest point of uncorrected astigmatism) fall on the retina, which can falsely increase the BCC value, leading to over-Add. The consequence of over-Add in progressive lenses is increased image distortion, narrower clear fields, and more difficult adaptation.
Patient's Experience in Singapore:
The patient mentioned that the optical shops in Singapore asked how the original prescription was obtained because it was a well-crafted prescription, except for the deteriorating coating in prolong used. Despite trying to match the prescription from the old Rodenstock lens card, the new lenses didn't work, and the patient tried multiple shops without success. Unfortunately, the patient didn’t bring the problematic glasses to the appointment, so I couldn’t determine the cause of the issue.
Personal Thoughts:
I believe modern lens technology should fully correct all refractive errors, making it unnecessary to stupid question like “how exactly or accuracy of a prescription should to prescribe ?. But Full Correction Exactly. But the problem is almose practitioner (on Thailand or some country) always use or rely the value from Auto-refractometer than retinoscopy because of Lazy or no skill in retinoscopy.
The question then arises: why do errors still occur in eye exams, even in developed countries like Singapore, despite advanced tools like wavefront aberrometers that can detect both lower and higher-order aberrations? In practice, these tools are often only useful for screening, not precise correction.
In contrast, a well-trained retinoscopy can achieve both accuracy and repeatability better than automated devices, though it requires skill. The reliability of retinoscopy lies in the ability to interpret the light reflected from the retina, accurately indicating refractive errors without deception (unless interpreted incorrectly). It can even be used in infants or animals to assess the clarity of the image on the retina (objectively) without needing verbal feedback (subjective test).
Left to ponder.
Just as the stethoscope is the essential tool for a physician, the retinoscope is the heart of optometry. An optometrist who cannot use a retinoscope is like a physician who cannot use a stethoscope.
Like a (Fake) Doctor who prescribes medication without understanding its side effects, an optometrist who prescribes glasses without considering the impact on binocular vision is equally problematic.
Hope you enjoy and thanks your your reading
Dr. Loft, O.D.

Contact Us
Loft Optometry ,578 Wacharapol Rd ,Tha-raeng ,Bangkhen , BKK 10220
mobile : 090-553-6554
line : loftoptometry
Additional Data : DNEye Scan 2
Product
Frame : Lindberg Spirit
Lens : Rodenstock B.I.G. Exact AllRound 1.6 with Solitire Lay-R x-clean